The Nutrient Shield: Warming Breast Milk Without Compromise

There is a very specific kind of quiet in the house when you are standing in the kitchen at 3:00 AM, baby on your shoulder, bottle in your hand, praying the milk warms just fast enough but not too hot. You worked hard for every ounce of that “liquid gold,” and the last thing you want is to damage its nutrients or make your baby uncomfortable.
As a mom who has stood in that exact darkness more than once, and as someone who now spends her days helping families navigate breastfeeding and baby gear, I want to reassure you: you can warm breast milk in a way that keeps it both safe and powerfully nutritious. Public health organizations such as the Centers for Disease Control and Prevention, La Leche League International, and HealthyChildren.org all offer guidance that fits beautifully with gentle parenting: respect your baby’s cues, protect their tiny body, and make your life easier, not harder.
This article will walk you through the key decisions you face: whether to warm milk at all, how warm it should be, which methods best protect nutrients, and what to do with thawed or leftover milk. Think of it as your nutrient shield blueprint, so every warm bottle supports your baby’s health and your peace of mind.
What Are We Protecting? The “Living” Power of Breast Milk
Breast milk is not just food; it is a living fluid. La Leche League International describes it as containing active immunological and bioactive components, and other medical sources echo that it is rich in antibodies, enzymes, white blood cells, and delicate proteins that support your baby’s immune system and development. Articles from Dr. Talbot’s Mom Blog and Kentec Medical point out that many of these components are heat sensitive. That means high or prolonged heat can denature proteins, decrease anti‑infective properties, and reduce fat quality.
Gentle warming, by contrast, aims to mimic milk coming directly from the breast, which is close to average body temperature around 98°F. Sources such as Dr. Talbot’s guides, Healthline, and several pediatric resources agree that warmed milk should feel lukewarm or comfortably warm, never hot. This is warm enough to be soothing for digestion and familiar for a baby who is used to nursing, but not so hot that it harms sensitive nutrients.
Imagine two pots of water on your stove. One is like a warm bath: pleasantly warm if you dip your wrist in. The other is boiling vigorously. When you set a bottle of milk into that gentler bath-like water for a few minutes, it gradually and evenly warms. In boiling water, the outer milk layers heat far too quickly, while the inside may still be cold. The research-based guidance from Elhée, Dr. Talbot’s articles, and La Leche League is clear: boiling or very hot water and microwaves are the enemies of breast milk’s living goodness.
Do You Even Need To Warm Breast Milk?
Here is the first big decision question many parents have: is warming breast milk required, or is it just a preference?
Several sources, including Momcozy, Mommed, Healthline, and Arizona Breastfed Babies, converge on the same answer. Healthy babies can safely drink breast milk cold, at room temperature, or warmed, as long as it has been stored and handled correctly. Cold milk from the refrigerator, or even slightly chilled milk from an insulated cooler, is fine from a safety standpoint. Many babies will accept cooler milk if they are introduced to it early and consistently.
So why do so many families still warm milk? Articles from Dr. Talbot’s Mom Blog and Momcozy highlight a few reasons. Warm milk mimics direct breastfeeding, which can make feeding more comfortable and efficient. Some babies latch and suck more steadily when the milk is close to body temperature, and a warm bottle in the evening can become a cue for winding down and sleep. Parents also report that warm milk seems to sit more softly on baby tummies, perhaps easing gas and fussiness.
There is one important nuance for tiny newborns and medically fragile infants. Pediatric guidance referenced by Baby Brezza’s educational content, citing Dr. Jacqueline Winkelmann, notes that serving cold breast milk or formula to newborns can lower their body temperature, increase oxygen use, and stress the body, showing up as fussiness, exhaustion, or tummy discomfort. For older, healthy babies, cold milk is usually fine; for newborns and vulnerable infants, it is worth checking with your pediatrician or NICU team about whether warming is recommended.
A practical example helps put this into perspective. If your three‑month‑old happily takes fridge‑cold milk at daycare, you do not need to fight that. In fact, it simplifies life for caregivers and reduces the risk of overheating. If your brand‑new baby shivers, grimaces, and refuses cold milk, gently warmed bottles near body temperature are likely worth the extra few minutes.
Core Principle: Warm Gently, Never Hot
Once you decide to warm, the next question is how warm. Several evidence‑based sources, including Momcozy, Parents magazine, Healthline, Kentec Medical, and AzBreastfedBabies, align on a simple idea: the sweet spot is around body temperature or a bit below. They describe this as roughly 98–104°F. Kentec Medical provides helpful temperature brackets for milk safety and comfort.
Here is a simple way to visualize the ranges, based on Kentec’s guidance and other pediatric sources:
| Milk temperature range | How it feels on your wrist | Typical use and notes |
| About 32–78°F (cold to cool) | Cool or cold to the touch | Safe if milk has been stored correctly; some babies are happy with this, especially older infants. |
| About 79–98.6°F (tepid to warm) | Slightly warm or “neutral,” not obviously warm | Good everyday feeding range; mimics milk that has cooled slightly after being expressed. |
| About 99–105°F (warm) | Comfortably warm but not hot | Still considered safe for nutrients and infant safety when tested carefully on the wrist. |
| 106°F and above | Hot on your wrist or uncomfortable to hold | Not recommended; heat at this level can damage beneficial components and raises burn risk for the baby. |
The wrist test, emphasized by Dr. Talbot’s guides, Healthline, the CDC, and many hospital systems, is wonderfully simple. After warming, place a few drops of milk on the inside of your wrist. It should feel lukewarm or comfortably warm, never hot or cold. If it feels too warm, let the bottle sit for a minute or two before trying again.
Notice that none of the trusted sources ask you to chase an exact number with a thermometer at home. They focus instead on gentle warming methods and the wrist test, with a shared warning against scalding heat and rapid, uneven warming such as microwaving.

Safe Warming Methods at Home That Protect Nutrients
The method you choose to warm breast milk matters just as much as the final temperature. Several breastfeeding‑focused brands, pediatric articles, and breastfeeding organizations all recommend variations of the same two methods: a warm water bath or a thoughtfully used bottle warmer with a gentle setting.
Warm Water Bath: The Trusted Classic
Dr. Talbot’s articles, Elhée’s breastfeeding journal, Healthline, Momcozy, and Arizona Breastfed Babies all describe the warm water bath as a tried‑and‑true method that preserves nutrients while avoiding hot spots. The concept is simple: you warm the water, and the water warms the milk.
In practice, you fill a bowl, mug, or small pan with warm tap water that feels like a comfortable bath on your wrist, not hot. You place the sealed bottle or milk storage bag in the water, making sure the water level stays below the cap or seal. Over about three to ten minutes, depending on volume and starting temperature, the milk gradually warms. Gently swirling the bottle midway helps distribute heat evenly and mix any separated fat without the rough agitation that can stress delicate components.
Many sources emphasize what not to do during a warm water bath. Do not use boiling water. Do not leave the bottle sitting in water that is uncomfortably hot to the touch. Do not place the bottle directly on an active burner or hot metal surface. La Leche League International, Elhée, and multiple pediatric hospitals all point out that very hot water and direct stove‑top heating can overheat the outer milk layers while the center remains cooler, damage bioactive proteins, and even melt or warp plastic bottles.
A real‑world example: you take a 4 fl oz bottle straight from the refrigerator at about 39–40°F and place it into a mug of warm tap water. After five minutes, you swirl gently and test a drop on your wrist. It feels just slightly warm. You have created body‑temperature milk without exposing it to harsh heat or uneven warming.
Bottle Warmers: Smart Help When Used Wisely
Bottle warmers are the baby‑gear equivalent of a slow cooker: they can be incredibly helpful when used correctly, and frustrating if misused. Dr. Talbot’s guides, Momcozy, Parents magazine, and several breastfeeding‑oriented brands all acknowledge their convenience, especially for nighttime feeds and pumping parents who warm bottles several times a day.
Not all warmers are created equal, though. Some use a warm water bath, which aligns with gentle warming recommendations. Others rely on steam, which heats faster and hotter. This distinction matters for breast milk. Baby Brezza’s educational content, for example, describes a “Steady Warm” mode that uses a warm water bath specifically designed to protect breast milk nutrients, and a separate “Quick Warm” steam mode intended for formula or baby food, which can tolerate higher temperatures.
Kentec Medical’s work with medical‑grade warmers in NICU settings goes even further. Their Koala Nutritional Warmer uses tight temperature control and feedback algorithms to prevent overheating human milk, with modes tailored to warming from fridge or freezer. The reason hospitals invest in this kind of precision is the same reason parents are urged to use gentle settings at home: vulnerable infants benefit enormously from preserving as much immunological power in milk as possible.
At home, this translates into a few simple habits. Choose a bottle warmer for breast milk that specifically mentions gentle or breast‑milk modes, follow the manufacturer’s instructions closely, and still test the milk on your wrist every time. AzBreastfedBabies cautions that many electric warmers heat too quickly or too hot; they even suggest using a quick‑read thermometer if you suspect your warmer overshoots. If the milk ever feels hot on your wrist or the bottle is unpleasant to hold, that is a sign to lower settings or return to a basic warm water bath.
A personal example from the trenches: with my second baby, we kept a small warmer on the nightstand. I preset it with a bottle of refrigerated milk in a basin of water before bed. When she stirred, I tapped the power button, changed her diaper, and by the time we were settled in the rocking chair, the bottle was warm but never steaming. That tiny bit of planning kept feeds gentle for her and sustainable for me.
Methods To Avoid Completely
Across all the reputable sources in this research—La Leche League International, the American Academy of Pediatrics, the CDC, Healthline, WIC Breastfeeding Support, and multiple hospital systems—one message is unwavering: do not microwave breast milk.
There are two main reasons. First, microwaves heat unevenly. Even if the bottle feels cool on the outside, the milk inside can develop hot spots that scald your baby’s mouth. Both the American Academy of Pediatrics and the CDC explicitly warn that uneven microwave heating can burn infants and that bottles can even explode if overheated. Second, microwaving at high temperatures damages breast milk’s living components. La Leche League cites research showing that high‑temperature microwaving significantly decreases anti‑infective properties, denatures bioactive proteins, and reduces fat content.
Direct stove‑top heating and boiling water baths have similar problems. Articles from Elhée, Parents magazine, and Arizona Breastfed Babies note that placing bottles in boiling water or heating milk directly over a burner makes overheating almost inevitable. High heat melts or distorts plastic, can bring milk into temperature ranges where antibodies and probiotic bacteria are damaged, and offers no nutritional advantage over a simple warm water bath.
If you have relied on the microwave in the past, this is not about guilt. You did the best you could with the information and energy you had. Going forward, shifting to a warm water bath or a gentle bottle warmer is one of the easiest, most powerful upgrades you can make to protect your baby’s milk.

On-the-Go Warming Without Losing Your Sanity
Leaving the house with a breastfed baby can feel like packing for a weekend trip. The BabyCenter community thread you saw in the research notes captures that feeling perfectly: pump before leaving, pack refrigerated bottles in an insulated lunch bag with ice packs, add a portable warmer, and suddenly your diaper bag weighs more than your baby.
The good news is that trusted sources such as Dr. Talbot’s Mom Blog, Mommed, WIC Breastfeeding Support, and the CDC all sketch out simple, flexible ways to warm milk on the go while staying within safe temperature and time limits.
One popular option is a portable bottle warmer. Many models are battery‑operated or USB‑powered and designed to work in a car cup holder or stroller caddy. Mommed describes them as compact devices that use water or controlled heat to warm bottles evenly. The key is the same as at home: follow the manufacturer’s instructions carefully, choose settings designed for breast milk rather than rapid steam, and always test the milk on your wrist.
Another low‑tech favorite is the thermos method described by Dr. Talbot’s guides. Before you leave home, you fill a high‑quality insulated bottle with warm water that feels like a comfortable bath on your wrist. When your baby is ready to feed, you place the sealed milk bottle in that warm water, swirl occasionally, and check the temperature after a few minutes. Because the thermos maintains a fairly stable temperature, you avoid the extremes of hot tap water or inconsistent restaurant kettles.
For longer outings, both the CDC and WIC Breastfeeding Support recommend transporting milk in an insulated cooler bag with frozen ice packs. In this setup, properly cooled milk can stay safe for up to about 24 hours. You might, for example, pack three 3 fl oz bottles in the cooler for a six‑hour trip, knowing your baby typically eats 2–3 fl oz every couple of hours, plus one extra small bottle as a buffer. When feeding time comes, you remove just one bottle from the cooler, warm it using your thermos or portable warmer, and keep the rest cold so their safety clock has not started yet.
In a pinch, Mommed even notes that body heat can help take the chill off slightly cool milk by tucking a bottle inside your bra or under your arm while you settle the baby. This is slow and best suited to milk that is already cool rather than very cold or frozen, but it is a gentle, no‑gear option when you are caught without warm water.
The overarching theme is to keep milk either cold in a cooler or gently warmed just before feeding, rather than letting it drift around at lukewarm room temperature for long stretches.

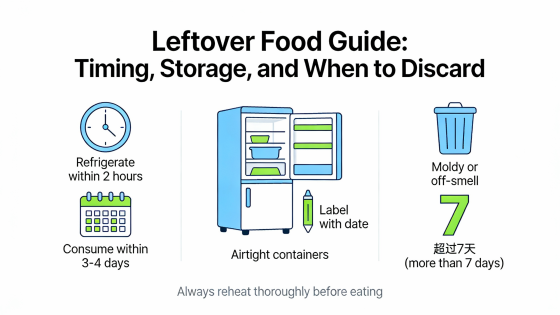
Timing, Storage, and When To Say Goodbye to Leftovers
The next big decision question is about time. How long can milk safely sit at different temperatures, especially after you have warmed it, and when must you let go of leftovers?
Before Warming: Safe Storage Windows
The CDC, WIC Breastfeeding Support, HealthyChildren.org, Wexner Medical Center, Mayo Clinic, and Medela all offer remarkably consistent guidelines for healthy full‑term babies, even though specific upper limits sometimes vary slightly depending on how cleanly the milk was expressed. A conservative, easy‑to‑remember pattern emerges.
Freshly expressed breast milk can stay at room temperature up to about 77°F for up to 4 hours, according to the CDC, WIC, and HealthyChildren.org. Some sources, such as Mayo Clinic and Medela, say up to 6 hours may be acceptable in very clean conditions, but they still prefer using or chilling within 4 hours, especially in warmer rooms.
In the refrigerator, most guidance converges on about 4 days at roughly 39–40°F. The CDC, Wexner Medical Center, and HealthyChildren.org all highlight that this timeframe is ideal when milk is stored in the back of the fridge rather than in the door, where temperatures fluctuate. Medela sometimes extends the window slightly under very clean conditions, but the “4 days” rule of thumb remains common and simple.
In the freezer, there is more leeway. The CDC, WIC, Wexner, and Mayo Clinic advise that breast milk is best used within about 6 months when stored at 0°F, but can be acceptable for up to 12 months if kept consistently frozen, especially in a deep freezer. Quality, particularly vitamin C levels and some subtle flavor notes, declines over time, but the milk remains safe when handled correctly.
For travel, the CDC, WIC, and several hospital systems agree that milk stored in an insulated cooler with frozen ice packs can be safe for up to about 24 hours. After you arrive, that milk should be used, refrigerated, or frozen promptly.
A simple scenario makes this concrete. If you pump at 7:00 AM and leave the milk on a cool kitchen counter, you ideally want it in the refrigerator by around 11:00 AM. If you know you will not use it within 4 days, you move it to the freezer, leaving some headspace in the container. When you pack for a day‑long outing, you place today’s bottles in a cooler with ice packs, confident that you have roughly a 24‑hour window from the time they went in.
Thawed and Warmed Milk: One‑Way Street
Once milk has been frozen and then thawed, or once it has been warmed, the clock speeds up. The CDC, WIC, La Leche League International, Medela, Nationwide Children’s Hospital, Dr. Talbot’s guides, and Vinmec’s article all emphasize that thawed and warmed milk are essentially one‑way tickets.
If you thaw frozen milk in the refrigerator, most sources recommend using it within 24 hours from the time it is completely liquid, as long as it stays in the fridge. La Leche League and Nationwide Children’s echo this 24‑hour guidance, and Medela offers similar timelines. WIC notes that thawed milk kept in the fridge should not be refrozen.
When you then warm that milk or allow it to reach room temperature, the window shrinks to about 2 hours. The CDC is very clear: once milk has been warmed or has reached room temperature, it must be used within 2 hours. Kentec Medical, Parents magazine, and several hospital guidelines align with this two‑hour window to limit bacterial growth.
Vinmec, focusing specifically on repeated reheating, goes even stricter. They recommend using warmed, previously frozen milk within about 1 hour and stress that it should not be reheated more than once. Their reasoning is that warm, protein‑rich milk is an ideal environment for bacteria, and each reheating cycle increases both bacterial growth and nutrient loss.
Leftover milk from a feeding is a special case. The CDC, Wexner Medical Center, and Nationwide Children’s generally say that if a baby has started drinking from a bottle, any remaining milk should be used within about 2 hours of the feeding and then discarded. HealthyChildren.org adds that any remaining milk should be used within 2 hours or, if quickly refrigerated, used for the very next feeding only. That nuance reflects real‑life situations where a baby pauses or naps mid‑bottle, but it is still a short window, not an invitation to keep reusing the same milk all day.
To make this more tangible, imagine you thaw a 4 fl oz bag in the fridge overnight. At 10:00 AM, you warm the milk and begin feeding. Your baby drinks 3 fl oz and leaves 1 fl oz in the bottle. You now have about 1–2 hours to either offer that leftover again or, if your pediatrician follows the HealthyChildren approach, quickly refrigerate it for the next immediate feed. After that, the safest choice is to discard it.
Planning smaller portions helps protect both safety and your pumping time. If your baby typically takes 3 fl oz per feed, storing milk in 2–3 fl oz portions means you may warm exactly what you need or combine two small bottles just before feeding. This reduces the odds of routinely throwing away full ounces of hard‑won milk.
Quick Reference: Time Limits Related to Warming
Drawing from the CDC, WIC Breastfeeding Support, HealthyChildren.org, Wexner Medical Center, and similar sources, here is a conservative overview of common time limits that relate directly to warming and feeding.
| Situation | Time limit (approximate) | Notes |
| Freshly expressed milk at room temp (≤ 77°F) | Up to 4 hours | Use or refrigerate as soon as reasonably possible. |
| Fresh milk in refrigerator (~39–40°F) | Up to about 4 days | Store in the back of the fridge; freeze sooner if not using within 4 days. |
| Frozen milk in freezer at 0°F or colder | Best within 6 months; acceptable up to 12 months | Quality (like vitamin C) slowly declines over time. |
| Milk in insulated cooler with frozen ice packs | Up to about 24 hours | Upon arrival, use, refrigerate, or freeze promptly. |
| Thawed milk kept in refrigerator (completely liquid) | Up to 24 hours | Never refreeze thawed milk. |
| Milk that has been warmed or is at room temperature | About 2 hours | Includes previously refrigerated or thawed milk once warmed. |
| Leftover milk after baby has started feeding | About 1–2 hours | After that, discard; HealthyChildren.org allows quick refrigeration only for the very next feeding. |
For premature or hospitalized infants, hospitals may use stricter rules, so always follow your NICU or pediatric team’s specific instructions.
Why These Cutoffs Matter
It can feel heartbreaking to pour leftover milk down the drain, especially when you remember the pumping sessions behind it. Understanding the “why” can make it a little easier to choose safety over salvage.
Bacteria thrive in warm, protein‑rich environments. Once milk leaves the sterile environment of a sealed, refrigerated container and especially once it touches your baby’s mouth, normal bacteria begin to multiply. Vinmec’s article highlights that repeated reheating of thawed milk significantly increases bacterial growth and can contribute to digestive upset or infections. Public health agencies like the CDC set conservative time limits to keep that bacterial growth in a safe range.
At the same time, each cycle of warming and cooling can slowly erode some of the delicate components that make breast milk special. La Leche League’s review of microwaving studies shows marked decreases in anti‑infective properties at high temperatures. While a single gentle warming in a warm water bath is not the same as microwaving, the principle is similar: minimal, one‑time warming helps preserve more of breast milk’s natural power.
Choosing Your Warming Setup for This Season of Motherhood
There is no single “right” way to warm breast milk for every family, and gentle parenting intentionally leaves room for your unique situation and your baby’s preferences.
In the newborn weeks, when you may be feeding very frequently and your baby is more sensitive to temperature changes, a simple warm water bath or a bottle warmer with a dedicated gentle or breast‑milk mode can be worth the investment. Having a predictable, safe routine can calm some of the stress of frequent nighttime feeds.
For an exclusively pumping parent heading back to work, the priorities shift toward organization and efficiency. Labeling each container with the date, storing in small 2–4 fl oz portions, using a “first in, first out” system as the CDC and WIC recommend, and keeping a warm water bath setup at home for evenings creates a smooth rhythm. At work, an insulated cooler with ice packs and access to a sink may be all you need.
If you mostly breastfeed directly and only occasionally pump for a date night or appointment, you may not need any special gear at all. A glass or silicone bottle, a mug of warm water, and a watchful wrist test line up perfectly with recommendations from Dr. Talbot’s Mom Blog, Elhée, and Healthline.
Your choice of bottles can play a role, too. Parents in the BabyCenter community mention that certain silicone bottles, such as ComoTomo, require compatible warmers or adapters. Elhée’s silicone bottles are designed to heat evenly in warm water baths and bottle warmers, while some parents prefer glass for its stability at warmer temperatures. Whatever you choose, the principles remain the same: gentle, even warming and careful time limits.

A Day in the Life: One Mom’s Warming Routine
To see how these principles fit together, imagine a day in the life of a mom of two. Her baby is 5 months old and takes three bottles while she is at work; her preschooler needs help with breakfast, socks, and a last‑minute show‑and‑tell treasure.
The night before, she pumps 9 fl oz of milk and divides it into three 3 fl oz bottles, labeling each with the date. The bottles go into the back of the refrigerator. In the morning, she packs them into an insulated cooler bag with two frozen ice packs, knowing from CDC guidance that they will stay safe for up to about 24 hours this way.
At daycare, the caregiver keeps the cooler closed between feeds. When it is time for the first bottle, they place one chilled bottle into a small container of warm tap water and swirl gently. After a few minutes, they test a drop on their wrist. It feels comfortably warm but not hot, matching the “lukewarm” target described by Dr. Talbot’s guides and Healthline. The baby finishes most of the bottle, leaving a tiny bit. The caregiver offers it again within about an hour and then discards the rest, in line with the two‑hour window recommended by the CDC and Wexner Medical Center.
At home that evening, the mom takes a bottle of milk she pumped two days earlier from the back of the fridge. She places it in the baby‑safe silicone bottle her baby prefers, sets it in a warm water bath on the counter, and sits on the floor to build block towers with her older child. After about five minutes, she swirls the bottle, checks the temperature on her wrist, and heads to the rocking chair. The milk is warm, the baby is calm, and she can relax knowing she has protected both nutrients and safety without adding complexity.

FAQ
Is it okay to feed my baby cold breast milk from the fridge?
Yes, for most healthy full‑term babies, cold or room‑temperature breast milk is safe as long as it has been stored correctly. Sources such as Momcozy, Mommed, Healthline, and Arizona Breastfed Babies all emphasize that warming is primarily about preference and comfort, not a strict medical requirement. Many babies, especially those introduced early to chilled bottles, do just fine with milk straight from the refrigerator.
There are two caveats. First, some babies genuinely prefer warm milk and may accept feeds more reliably when the milk is close to body temperature. Second, pediatric guidance cited by Baby Brezza and Dr. Jacqueline Winkelmann notes that cold milk may lower body temperature and increase oxygen use in newborns, potentially leading to fussiness or fatigue. If your baby is premature, has medical conditions, or is still in the newborn stage, it is wise to ask your pediatrician whether they recommend warming milk for now.
If my baby likes very warm milk, will that destroy nutrients?
Babies who clearly relax and drink more enthusiastically with warmer milk are telling you something important about their comfort. You can honor that while still protecting the milk’s nutrients. Research‑informed sources such as Kentec Medical, Momcozy, Healthline, and Parents magazine describe a broad safe range for warmed breast milk that tops out around 104–105°F. Within that range, the focus is on avoiding obvious heat and hot spots, not hitting a precise number.
In practice, this means aiming for milk that feels comfortably warm on your wrist but never hot. If it feels even slightly too warm to leave on your skin, it is too hot for your baby’s mouth and may start to creep into temperatures where protective components break down more quickly. Letting the bottle cool for a minute, swirling it again, and retesting is a simple way to stay in the safe zone while still serving milk that your baby finds soothing.
Can I refrigerate and rewarm leftover milk from a bottle?
This is an area where guidance is cautious, because it involves both bacterial growth and nutrient changes. The CDC, Wexner Medical Center, and Nationwide Children’s Hospital generally recommend using leftover milk from a feeding within about 2 hours and then discarding it, rather than cooling and reheating multiple times. Vinmec strongly warns against repeated reheating of thawed milk because of increased bacterial growth and potential digestive issues.
HealthyChildren.org notes that any remaining breast milk after a feeding should be used within 2 hours or, if quickly refrigerated, used for the next feeding. That is a very short, one‑time extension, not a full extra day of use. Since recommendations can vary slightly, the safest approach is to treat warmed milk and partially used bottles as short‑window feedings, and to ask your pediatrician which policy they prefer for your baby, especially if your baby was born prematurely or has health complications.
A practical way to minimize waste is to store and warm milk in smaller 2–4 fl oz portions, as suggested by the CDC, WIC Breastfeeding Support, HealthyChildren.org, and Mayo Clinic. You can always warm a bit more if your baby surprises you with a bigger appetite, but you cannot safely undo over‑generous portions once a bottle has been warmed and used.
Can I thaw frozen milk at room temperature to save time?
Thawing at room temperature for long periods is not recommended. The CDC, La Leche League International, WIC Breastfeeding Support, Medela, and Nationwide Children’s all recommend slow, gentle thawing in the refrigerator or faster thawing under lukewarm running water or in a container of warm water. These approaches keep milk out of the temperature range where bacteria multiply fastest for as long as possible.
A realistic compromise is to plan ahead when you can. Moving tomorrow’s milk from freezer to refrigerator the night before lets it thaw gradually over 12–24 hours. If you forget or plans change, holding the sealed container under warm running water or using a warm water bath for a few minutes will thaw it more quickly without the risks of room‑temperature thawing or microwaving. Once fully thawed, remember to use it within about 24 hours and never refreeze it.
A Gentle Closing Thought
You do not have to chase perfection to protect your baby’s milk; you only need a few steady, evidence‑based habits. Warm gently, never hot. Respect the time limits. Swirl instead of shake. And give yourself as much compassion as you give your baby. Every careful choice you make around that little bottle is an act of love, and that love is just as nourishing as the milk itself.
References
1. https://t.gsu.edu/3V05Umz
2. https://wicbreastfeeding.fns.usda.gov/storing-and-thawing-breast-milk
3. https://www.canr.msu.edu/news/safely-warming-up-baby-formula-and-breastmilk
4. https://wexnermedical.osu.edu/our-stories/breast-milk-storage
5. https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=90&contentid=p02682
6. https://www.cdc.gov/breastfeeding/breast-milk-preparation-and-storage/handling-breastmilk.html
7. https://med.stanford.edu/newborns/professional-education/breastfeeding/storage-and-shipping.html
8. https://ukhealthcare.uky.edu/obstetrics-gynecology/obstetrics/breastfeeding-support/storing-warming-milk
9. https://health.usf.edu/-/media/v3/usf-health/COPH/Research/Chiles-Center/FPQC/MOM-Resources/PumpingandMilkStorage.ashx
10. https://healthonline.washington.edu/sites/default/files/record_pdfs/Breastfeeding-06-Expressing-Storing-Breast-Milk.pdf




